Scientists at Zhejiang University have found that they have been approved for diabetes or can treat fatal breast cancer
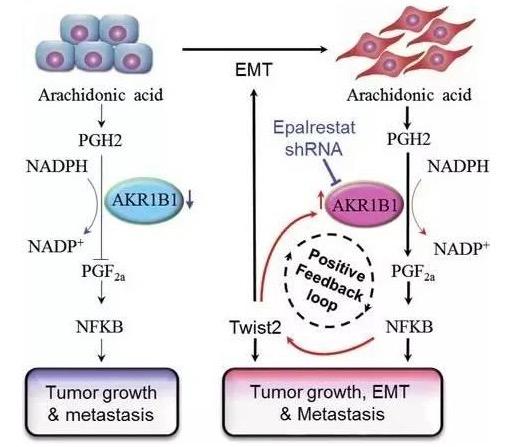
Scientists at Zhejiang University have found that they have been approved for diabetes or can treat fatal breast cancer March 24, 2017 Source: Singularity Network According to WHO statistics, about 1.2 million women worldwide suffer from breast cancer every year, and 500,000 women die of breast cancer. Basal-like breast cancer is a very dangerous form of breast cancer. It is highly invasive and can spread rapidly or metastasize to the brain and lungs. Because no effective drugs have been found, the mortality of patients with basal breast cancer is extremely high. Scientists have been looking for effective treatments. In recent years, studies have shown that there is a certain correlation between diabetes and breast cancer. There are many treatments and drugs for diabetes. Is there a way to treat basal-like breast cancer? The research team of Professor Dong Chenfang from Zhejiang University in China finally found the answer. They found that in basal-like breast cancer cells, there is an enzyme called AKR1B1 that is extremely active. This enzyme can indirectly "liberate" cancer cells, allowing cancer cells that were originally stuck in a non-movable cell to become large and can be used in patients. The body is free to flow. This is also a big reason for the danger of this cancer. It is also a coincidence that AKR1B1 is one of several diabetes-related genes that have been identified. Some of the AKR1B1 enzyme inhibitors currently used to treat diabetes, such as the drug epalrestat, may become effective targets for the treatment of fatal breast cancer. This important research result of Professor Dong Chenfang's team was published in the famous medical journal Journal of Experimental Medicine on March 7. In fact, the process by which AKR1B1 "liberates" cancer cells is through the process of epithelial-mesenchymal transition (EMT), the transformation of epithelial cells that do not have the ability to exercise into mesenchymal cells with exercise capacity. This process is involved in the formation of cancer stem cells and the infiltration, migration and metastasis of tumor cells during the development of cancer. In other words, the important step in the development of cancer and metastasis of cancer cells is the epithelial-mesenchymal transition process. Epithelial-mesenchymal cell transformation (from a square "good family" cell to a "pointed tip brain" malignant cell) Through the preliminary experiments, Dong Chenfang's team found that the expression of AKR1B1 in basal-like breast cancer cells was significantly higher than other breast cancer subtypes. To test this connection, the researchers attempted to knock down the AKR1B1 gene in basal-like breast cancer cells. As a result, when the AKR1B1 protease was decreased in the cells, the intracellular E-cadherin (the "binder" between the cells) was significantly increased, and the cells were more firmly fixed. When the AKR1B1 protease is increased, the E-cadherin is reduced and the binding to the cells is reduced. Therefore, it can be shown that AKR1B1 does play an important role in inducing migration and invasion of basal-like breast cancer cells. This just verifies the link between AKR1B1 and basal-like breast cancer and does not explain anything. The key to the problem is coming! To further explore the functional mechanisms of AKR1B1 and epithelial-mesenchymal transition, the researchers pointed to Twist2. Because Twist2 is known to play a crucial role in epithelial-mesenchymal cell transformation. Studies have also shown that Twist2 is significantly expressed in basal-like breast cancer cells, but not in normal breast cancer cells. Sure enough, the team's researchers found that the expression of AKR1B1 is actually induced by the cellular transcription factor Twist2. Even more surprisingly, AKR1B1 expression further increased Twist2 levels by producing prostaglandin F2 that activates the NF-B signaling pathway. Thus, during epithelial-mesenchymal cell transformation, Twist2 induced AKR1B1 expression, and AKR1B1 increased Twist2 levels. It is this "positive feedback loop" that plays a powerful role in promoting the transformation of basal-like breast cancer cells through epithelial-mesenchymal cells. Thinking about the fast-fat and high mortality of basal-like breast cancer, I can't help but feel a little stunned. The following figure is a mechanism model discovered by the researchers that "AKR1B1 promotes basal-like breast cancer by a positive feedback loop that activates the EMT procedure." AKR1B1 regulates EMT through a positive feedback loop leading to tumorigenicity and metastasis model As mentioned at the beginning of the article, this finding means that AKR1B1 inhibitors can not only cure diabetes, but also serve as an effective targeted drug for the treatment of basal-like breast cancer. To test this bold conjecture, the researchers went on to do a series of rigorous experiments: First, the results of AKR1B1 knockdown expression in an ex vivo environment were verified by in vitro culture experiments of human basal-like breast cancer cells. It is very exciting that knockdown of AKR1B1 expression or administration of epalrestat can significantly reduce the number of basal-like breast cancer cell colonies (because the cells are free, they go to each play), while in AKR1B1 In the expressed cells, the formation of colonies was significantly increased. The researchers then transferred the experiment to the mouse. The results showed that administration of epalrestat could significantly inhibit tumor growth in mice; in non-administered mice, tumor growth was evident in vivo due to the expression of AKR1B1. Finally, the researchers tested whether inhibition of AKR1B1 expression would affect tumor metastasis. The results are equally striking, giving epalrestat, reducing AKR1B1 activity, and greatly inhibiting lung metastasis of cancer cells in vivo. The results of the experiments have fully demonstrated that AKR1B1 inhibitors can well prevent the metastasis and invasion of human basal-like breast cancer cells in vitro and in mice. More importantly, epalrestat, a drug that inhibits AKR1B1 activity, has been approved by Japan for the treatment of peripheral neuropathy associated with diabetes. Professor Dong Chenfang said: "In view of the fact that epalstat has been sold in the market and there are no major side effects, our research provides a basis for the most valuable use of epalrestat for clinical treatment of basal-like breast cancer. Targeted drugs." Shenzhen Sunson Tech Co., Ltd , https://www.sunsonkiosk.com